"Coconut oil INDUCES ENDOTOXEMIA IN DOGS."
"Coconut oil causes LEAKY GUT IN DOGS"
"Coconut oil is PRO-INFLAMATORY."
Are these claims true or false? The answer: False! Read on to learn why.
These false claims about coconut oil were actually made in the news, perpetuating yet again, more negative misinformation about coconut oil.
Within a two-day period, I’ve been contacted by a well-known animal health blogger and influencer, a certified animal nutritionist, an integrative vet, and a slew of very concerned pet parents…
So, what's all the fuss about?
Recently, a vet made a post on Facebook about a podcast that discussed endotoxemia and leaky gut syndrome in dogs. And here's the kicker – the podcast is packed full of inaccuracies and misinformation about coconut oil.
The interviewee is a microbiologist who's knowledgeable on gut microbiome and gut bacteria. However, his knowledge on fats and fat metabolism is completely inaccurate. Here are a few of his erroneous and contradictory "facts":
- Because coconut oil is “predominantly a long chain fatty acid (LCFA)”, it promotes the increase of an endotoxin called lipopolysaccharides (LPS) in the blood
- Coconut oil is one of the biggest drivers of endotoxemia in dogs.
- When coconut oil is digested, it forms chylomicrons which transport endotoxins into the circulatory system leading to chronic systemic inflammation
These statements are inaccurate and misinformed. And needless to say, the interview caused a lot of panic.
Here's what the science says:
- Coconut oil is about 63% medium-chain fatty acid (MCFA), and contains only an average of 37% long chain fatty acids (LCFAs)
- Medium-chain fatty acids (MCFAs) in coconut oil are not converted to chylomicrons (no fat is converted into chylomicrons)
- Chylomicrons are lipoproteins that carry fat, protein, and cholesterol from the digestive tract throughout the body for redistribution
- Chylomicrons are formed inside the intestinal wall
- Few MCFAs, if any, are incorporated into chylomicrons
- MCFAs are absorbed into the portal vein and sent directly to the liver where they are either utilized to produce energy or converted into ketones
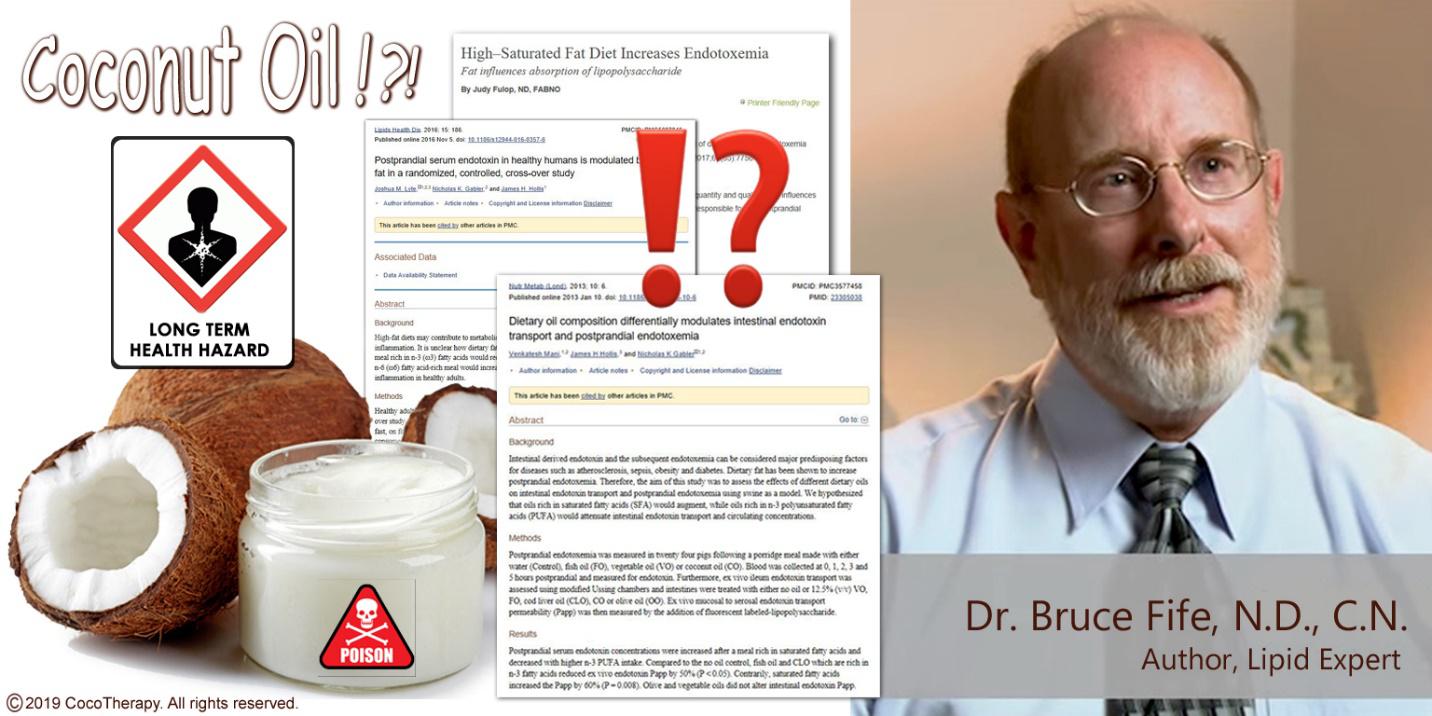
I decided to reach out to my friend and foremost expert on fats and coconut, Dr. Bruce Fife, ND, CN, to dig deeper and get the real scientific facts on coconut oil and its effects on endotoxins and inflammation. I sent him the link to the interview, as well as some published studies on this topic.
The interview
Below is our comprehensive discussion about this subject.
Charisa: Bruce, there’s a study on coconut oil that has surfaced on social media and the news, and it’s causing a lot of controversy and confusion among animal lovers who feed coconut oil to their dogs. It basically states that coconut oil can increase endotoxemia in dogs and increase the absorption of lipopolysaccharides, causing chronic inflammation. You may have heard of these studies.
Bruce: Charisa, thank you for contacting me about this issue and providing the links. I have had a few others mention this issue as well.
Charisa: Before we jump into the interview and studies, I can’t help but notice --- when it comes to saturated fat studies, why do researchers use coconut oil as their source of saturated fat? Why not use a more commonly consumed saturated fat, such as beef or butter fat?
Bruce: Sometimes researchers use coconut oil as the source of saturated fat because it has a higher percentage of saturated fatty acids than other fats, including animals’ fats. But unlike animal fats, coconut oil is composed predominately of medium-chain fatty acids (MCFAs). Much of the confusion about coconut oil and endotoxemia stems from a study published in the journal Nutrition and Metabolism titled “Dietary oil composition differentially modulates intestinal endotoxin transport and postprandial endotoxemia.” Others have used this study as the basis for their criticism of saturated fats and coconut oil. However, there are some concerns about the study.
First, it appears that the authors of this study are inherently anti-saturated fat and also anti-coconut oil. They indicated this by their opening statement that they hypothesized that saturated fat (coconut oil in this case) would cause inflammation and thus promote inflammatory diseases and that polyunsaturated oils would not. So, there is an inherent prejudice before the study was ever conducted. This suggests that the study was conducted to prove the author’s point of view rather than to uncover scientific truth.
Second, why did they choose coconut oil to test as a saturated fat and not butter or beef fat? Coconut oil is unique and unlike animal fats, and far less often consumed. It appears they chose coconut oil for a specific reason.
Charisa: Well, it’s very apparent that these researchers don’t make any distinction on the types of saturated fats. They lump all saturated fats in the same bucket --- long-chain and medium-chain fats. Why do you think this is done?
Bruce: These researchers did not explain why they used coconut oil as their source of saturated fat. And the fact that they make no distinction on the types of saturated fats is a major problem in the first place. MCFAs are very unique, and are used in the body very differently from LCFAs. This is quite common in nutritional research -- designing a study to achieve the outcome you desire. In this case, to find evidence to cast criticism and doubt on saturated fat in general, and coconut oil in particular. I believe they chose coconut oil for its high MCFA content and its associated antimicrobial properties.
Charisa: Let’s talk about the author’s claim that coconut oil is pro-inflammatory. I’ve always believed that coconut oil is anti-inflammatory! Why would they say that?
Bruce: Although they claim it is pro-inflammatory, coconut oil has shown to be anti-inflammatory in other studies. They alluded to the possible danger of using coconut oil for Alzheimer's, saying it promotes the development of plaque. However, other studies have shown that coconut oil actually reduces the formation of plaque in the brain and improves brain function in Alzheimer's patients. Hundreds of testimonials also support these findings.
Keep in mind that coconut oil is predominately composed of MCFAs -- all of which are saturated fats. Mother's milk is a good source of MCFAs. Something like 60% of the fat in mother's milk is saturated. Did nature purposely put MCFAs and other saturated fats in milk to kill infants? All mammals' milk contains MCFAs and is high in saturated fat. If saturated fat was so deadly why are we alive? How did we ever survive childhood when saturated fat-rich milk was our only food? These scientists don't look at the obvious!
Charisa: We know that MCFAs contain potent anti-bacterial, anti-viral, anti-microbial properties. We also know that it supports a healthy immune system. Is there a connection between bacteria die-off and an increase in inflammation? How does it function when babies drink mother’s milk, which is full of saturated MCFAs?
Bruce: MCFAs perform many vital functions in milk and are considered conditionally essential fatty acids--meaning they are essential during infancy, we must have them when young in order to avoid deficiency symptoms and grow and develop as nature intended. Some of these functions are to protect us from infections and to train our immune system to recognize potential threats and quickly deal with them. MCFAs kill disease-causing bacteria in the gut. Some fragments of these dead bacteria can be absorbed into the intestines and into the bloodstream. Here they activate a mild immune response which trains the infant's immune system to recognize a bacterial threat and mount a defense without the actual threat of an infection (the bacteria are already dead).
Charisa: I’ve always believed that coconut oil does not produce chylomicrons as it goes directly through the portal vein to the liver. And because of this, it cannot transport the endotoxin, lipopolysaccharide (LPS) through the circulatory system. Is this true or am I missing something?
Bruce: In general, you are correct. However, the process is not perfect. Most MCFAs are absorbed through the portal vein but some are still absorbed into the intestines. What few MCFAs that are not absorbed into the portal vein are absorbed by the cells lining the intestinal wall. MCFAs pass through the cell membrane into the cells themselves and are used as fuel to produce cellular energy. Very little, if any, ever get incorporated into chylomicrons.
Chylomicrons are formed in the intestines and are filled with whatever type of fatty acids are available, almost always LCFAs. They will also absorb fragments of LPS--bacteria cell membrane from dead bacteria killed by MCFAs. This is how gut LPS gets into the bloodstream.
Charisa: Let’s talk about the endotoxin, lipopolysaccharide (LPS). How does it cause inflammation?
Bruce: LPS, which is derived from the membrane that encases gram negative bacteria, initiates an immune reaction. The immune system identifies LPS as an invading bacteria and attempts to dispose of it. This process involves an inflammatory reaction to speed white blood cells to the LPS to get rid of the invader. This is a temporary action. Once the LPS is taken care of, inflammation stops. This is how the body normally protects itself. It is a positive short-lived response to a threat.
The authors of this study point out that high blood levels of LPS are associated with systemic inflammation. This is especially true when the LPS is associated with living bacteria that are invading the body. An inflammatory response is essential to remove the infection and prevent death.
Charisa: And can MCFAs transport LPS into the circulatory system?
Bruce: MCFAs do not transport LPS themselves. They only produce fragments of LPS that are small enough to be absorbed into the intestinal wall -- a normal healthy intestinal wall. It does not have to be a compromised leaky gut. This is how MCFAs in mother's milk trains the infant's immune system to recognize danger and respond appropriately.
Absorbing LPS is not a disease or a mistake of nature but part of the perfect design of nature. It serves a vital function. These scientists are twisting the facts to make coconut oil/saturated fat a villain when it is doing what it is designed to do to keep us healthy. Coconut oil can increase the amount of LPS in the bloodstream because it is killing these harmful bacteria in the gut and fragments of the dead bacteria can be absorbed via the chylomicrons into the bloodstream.
Charisa: What about the studies that state that MCFAs from coconut oil increase blood levels of LPS?
Bruce: It has been seen that some fats, primarily MCFAs, increase blood levels of LPS. Not bacteria but just the LPS -- fragments of dead bacteria. This is because MCFAs kill harmful bacteria in the gut and fragments of LPS are absorbed into the bloodstream.
In an effort to blame saturated fat as the cause of various health issues, some people have claimed that eating saturated fat (in this case coconut oil) causes an increase in LPS and, therefore, may possibly cause systemic inflammation. If saturated fat is consumed frequently, then it would theoretically promote chronic inflammation and, therefore, promote inflammatory diseases such as atherosclerosis, diabetes, autoimmune diseases, etc. If this were true, it would mean that saturated fat might indeed contribute to the development of heart disease because it is now accepted that inflammation is the primary cause of arterial plaque and, consequently, heart attacks and strokes, and not excess cholesterol.
The LPS that is absorbed after eating coconut oil or other saturated fats does not produce a strong enough or long lasting enough immune response to cause chronic inflammation or promote inflammatory disease. It is chronic inflammation that leads to inflammatory disease, not transitory inflammation that the body uses to protect itself from infection. A study published in the journal Lipids in Health and Disease titled “Postprandial serum endotoxin in healthy humans is modulated by dietary fat in a randomized, controlled, cross-over study,” Investigated the inflammatory effect of LPS from coconut oil. While the increase in blood LPS resulting from the ingestion of coconut oil does initiate an immune response, an increase in inflammation was undetectable. Therefore, coconut oil could not promote inflammatory diseases.
As I mentioned earlier, if MCFAs did promote chronic inflammation, then mother’s milk, which is a rich source of both MCFAs and saturated fat, would cause great harm to infants that consume only milk, the same goes for all mammals, including our pets. Mothers don’t produce milk to kill off their young. Carnivores, including dogs and cats, and many omnivores, which consume diets very high in saturated fat, normally do not suffer from inflammatory diseases. The idea that LPS from saturated fats cause chronic inflammation is absolutely absurd.
Charisa: Bruce this is a lot of fascinating information. And while it all makes sense, scientifically --- sometimes people forget to see the forest through the trees, take studies out of context, and only look at one part of a process. Can you, in couple of sentences, quickly summarize why people don’t have to be afraid of coconut oil increasing chronic inflammation?
Bruce: While coconut oil does raise LPS, it does not instigate a measurable rise in systemic inflammation and, therefore, does not contribute to inflammatory diseases. The LPS is from dead bacteria so there is no threat of an infection and no need for a robust inflammatory response. As I’ve said, absorbing LPS is not a disease or a mistake of nature, but part of the perfect design of nature.





My deepest thanks to Dr. Bruce Fife for taking the time to talk to me about this topic.
For more information on how coconut oil can protect the body from inflammatory disease, please see: "The Protective power of Dietary Fat: Fatty Acids and Immune Function", by Dr. Bruce Fife, N.D.C.N.: http://coconutresearchcenter.org/hwnl_16-4.htm
About Dr. Bruce Fife:
Dr. Bruce Fife, N.D.C.N., is an author, speaker, certified nutritionist, and naturopathic physician. He has dedicated his life to studying lipids and coconut oil, and has written over 20 published books, hundreds of articles, and has reviewed hundreds of scientific and medical research studies related to fats, coconut oil, and its effects on humans and animals. He is the publisher and editor of the Healthy Ways Newsletter and serves as the president of the Coconut Research Center, a non-profit organization whose purpose is to educate the public and medical community about the health and nutritional aspects of coconut and related foods. Dr. Fife is considered one of the world's leading experts on the health aspects of dietary fats and oils. He is a popular speaker and travels throughout the world lecturing at universities, trade shows, conferences, hospitals, and spas. He has appeared on hundreds of radio and television programs worldwide.